How to Plan Mammography Exams Around COVID-19 Vaccines
Now that mass vaccinations against COVID-19 are underway, Desert Imaging has issued new guidance in accordance with the Society of Breast Imaging (SBI) on how to coordinate mammography exams for patients who plan to receive or have recently received a Covid-19 vaccine.
According to the SBI, “women with a recent COVID-19 vaccine may present for diagnostic workup for newly palpable axillary adenopathy or have new axillary adenopathy identified on routine screening mammography or ultrasound.” In other words, the lymph nodes located under the arm may enlarge on the side in which the vaccine was injected as a natural immune system response. The lymph nodes are part of the white blood cells or infection fighting system of the body. Vaccines of all types can result in temporary swelling of the lymph nodes, which may be a sign that the body is making antibodies in response as intended.
However, the detection of the enlarged lymph nodes may result in additional imaging to make sure everything is in order. To reduce the probability for additional imaging, Desert Imaging’s guidance to Mammography patients is as follows:
For Annual Screening Mammograms
If the patient has not yet received a COVID-19 vaccine, please schedule the screening mammogram before receiving the first dose of a vaccine.
If the patient recently received a COVID-19 vaccine, please schedule, or reschedule the screening exam 4-6 weeks after the date of the final COVID-19 vaccine.
For Diagnostic Mammograms
No delay if the patient needs to schedule a diagnostic mammogram. Notation will be made of the vaccination dates and location of the injection.
Desert Imaging strongly encourages our patients and the El Paso community to receive a COVID-19 vaccination as soon as one becomes available to them. We are happy to adjust our imaging schedules to accommodate the needs of our patients and to deliver the most accurate imaging results as possible. Please feel free to contact us at (915) 577-0100 or www.DIELP.com if you should have any questions or concerns.

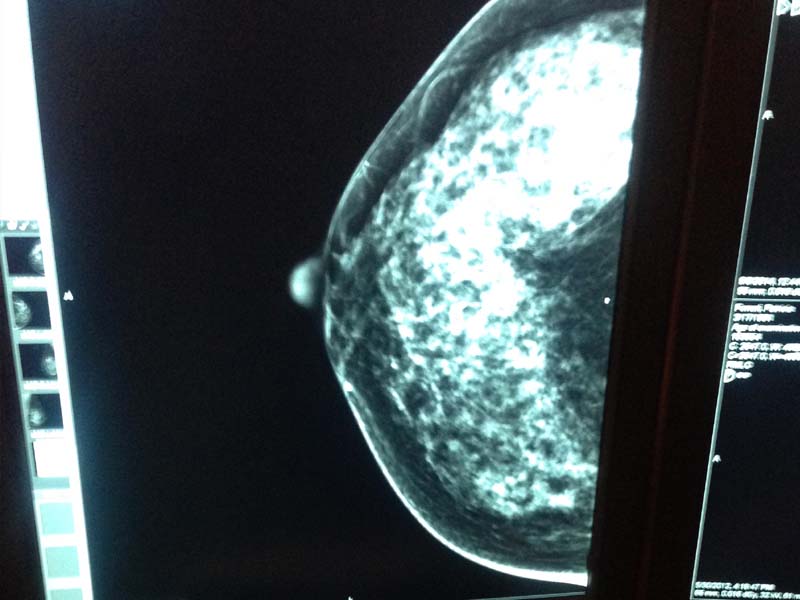
The image above is a side-by-side comparison of a mammogram. The oval bean-shaped structures are the lymph nodes under the arm. The image on the right was taken in 2015 in which the lymph nodes appear normal. The image on the left was taken two days after the second dose of the COVID-19 vaccine in which the lymph nodes appear enlarged.
Peace of mind
At Desert Imaging, we provide peace of mind during your entire mammography or imaging experience. Our compassionate staff creates a warm and welcoming environment to ease the anxiety often associated with getting a mammogram. Our team at our Desert Imaging is highly trained clinically but are also trained in the art of putting patients at ease. We do everything possible to make each experience an exceptional one.
The accuracy provided by our breast health experts and state-of-the-art technology is increased by the specialized breast expertise of our dedicated staff. Our caring and compassionate team provides personalized, attentive care for everyone who walks through our doors. Understanding that waiting for your results is also part of the experience, we strive to make your wait as short as possible. Results are delivered via secure fax to your provider, usually within 24 to 48 hours.

3D Digital Mammography
The Genius™ 3D Mammography™ exam, available on the Selenia® Dimensions® system from Hologic, is available at three Desert Imaging clinics across El Paso: (East) 1727 Lee Trevino Drive 79936, (Far East) 3080 Joe Battle, and (West) 122 W. Castellano Drive 79912. These systems expand Desert Imaging’s comprehensive commitment to promoting breast health in the region when coupled with our existing breast services including breast MRI, ultrasound, biopsy, and elastography.
The Importance of the 3D Mammogram
Just Ask Sheryl Crow

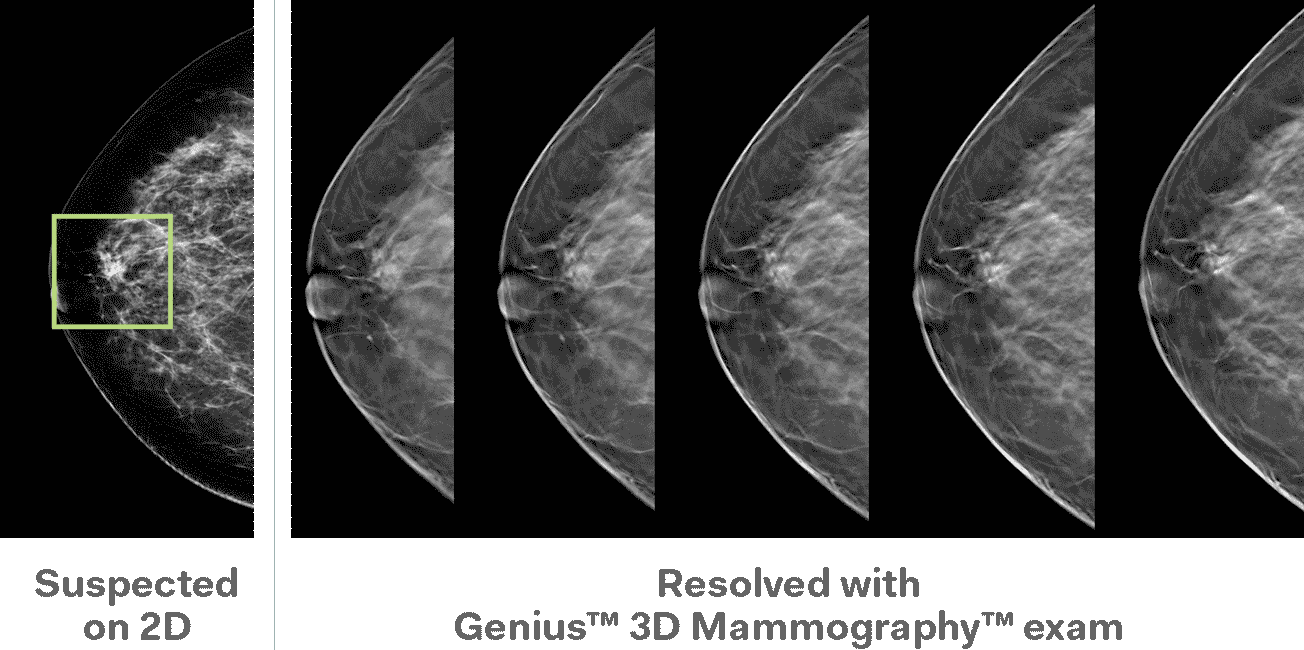
Case Study 2D vs 3D
A conventional x-ray examination of the breast, called a mammogram, is two-dimensional (2D): two x-ray images are taken of the breast, from top-to-bottom and from angled side-to-side, while the breast is compressed between a clear plastic paddle and an imaging detector. Although compression is necessary to obtain breast images, it may cause overlapping of the breast tissue in which abnormal tissue can be hidden and superimposed normal tissue can appear abnormal.
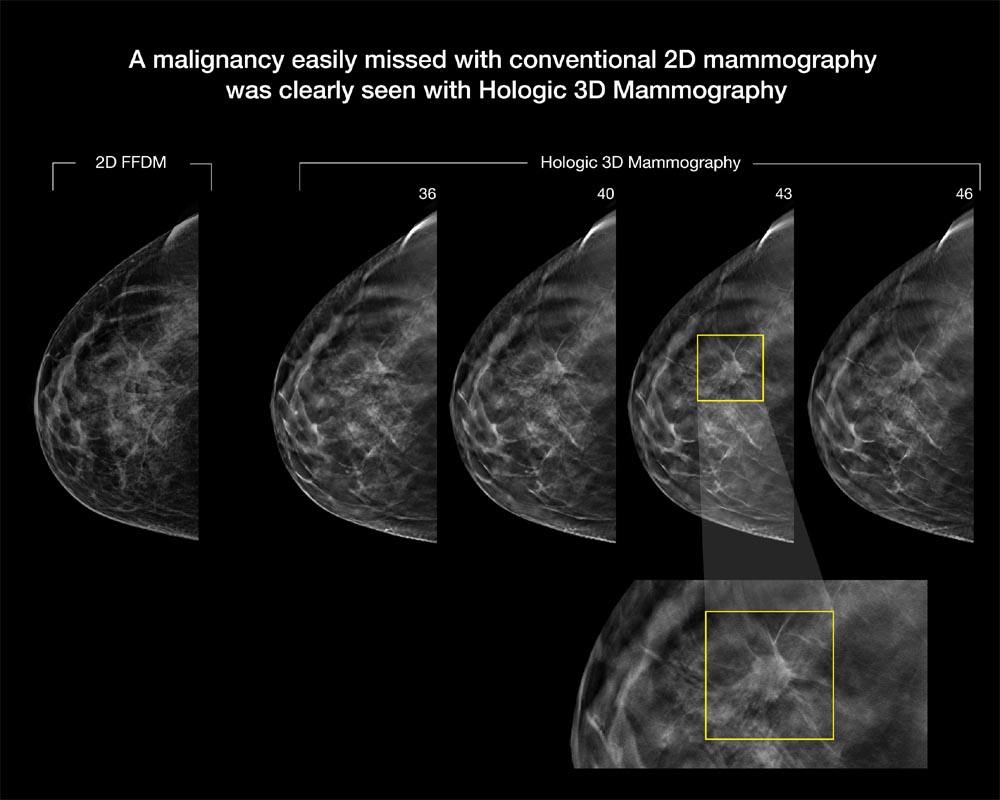

Breast tomosynthesis
Breast tomosynthesis is an advanced form of breast imaging that uses a low-dose x-ray system and computer reconstructions to create three-dimensional images of the breasts. During this 3D exam, the x-ray arm sweeps in a light arc over the breast, taking multiple images. A computer then converts the images into a stack of thin layers, allowing the radiologist to review the breast tissue one layer at a time. This process minimizes the tissue overlap that can hide cancers or make it difficult to distinguish normal overlapping breast tissue from tumors. It also requires no additional compression and virtually the same imaging time as a conventional 2D breast cancer screening exam.
Full Field Digital Mammography
At Desert Imaging, we are all about Mammography. We only use full field digital mammography which is the Gold Standard because the image quality is unsurpassed. At Desert Imaging, all 3 stand alone locations and all our MOM Units, (Mammos on the Move, Mobile Mammogam Coaches) use Hologic Selenia.
Insurance
Most insurances cover mammography at 100%, no cost to you. The diagnostic mammogram, however, will be charged the copayment or the deductible.

Screening mammogram
A screening mammogram is comprised of 4 images, 2 of the right breast and 2 of the left. The screening images can show the radiologist if the breast is free of calcifications or mass structures. The radiologist can tell if the mammogram is normal (negative) or benign (may have cysts, masses, or calcifications that are not suspicious).
Diagnostic mammogram
A diagnostic mammogram is needed if the radiologist needs to take a closer look at cysts, masses, or calcifications that look suspicious. These diagnostic images can help the radiologist tell if something is malignant or not. If they are still questionable, a biopsy might be ordered to look directly at the tissue.
What you should know about
HENDA'S LAW
What is Henda's Law & how does it affect my mammogram?
Henda's Law is the informal name for a House Bill passed by Texas Legislature that requires mammography providers to inform women that dense breast tissue can affect the accuracy of a mammogram in detecting breast cancer.The bill was initiated by Henda Salmeron, whose breast cancer went undetected because routine mammograms did not pick up the cancerous tumors hiding behind her dense breast tissue. Women, like Henda, who have dense breast tissue may benefit from supplemental screening.
Do I have dense breast tissue?
Breast density refers to the amount or ratio of fibroglandular to fatty tissue. As a woman ages, fibroglandular tissue is replaced by an increase in fatty tissue and thus making breast cancer more readily visualized on a mammogram.

How will this affect my annual exam?
If a physician notices you have dense breast tissue, additional exams such as ultrasound may be ordered to rule out the possibility of any hidden tumors. However, it is important that you know insurance may not cover these additional screenings at 100%.
BIRADS
The American College of Radiology (ACR) came up with a standard way to describe mammogram findings and results. In this system, the results are sorted into categories numbered 0 through 6. This system is called the Breast Imaging Reporting and Data System (BI-RADS). Having a standard way of reporting mammogram results lets doctors use the same words and terms, which can help ensure better follow up of suspicious findings. These categories are used in the official report that goes to your doctor. Different wording may be used in the letters sent to patients. Here’s a brief review of the categories:
Additional imaging evaluation and/or comparison to prior mammograms is needed.
This means a possible abnormality may not be clearly seen or defined and more tests are needed, such as the use of spot compression (applying compression to a smaller area when doing the mammogram), magnified views, special mammogram views, or ultrasound. This may also suggest that the mammogram should be compared with older ones to see if there have been changes in the area over time.Negative
There’s no significant abnormality to report. The breasts look the same (they are symmetrical) with no masses (lumps), distorted structures, or suspicious calcifications.Benign (non-cancerous) finding
The radiologist describes a finding to be benign, when he/she sees benign, non malignant, structures such as, calcifications, lymph nodes in the breast, benign cysts or calcified fibroadenomas. This ensures that others who look at the mammogram will not misinterpret the benign finding as suspicious. This finding is recorded in the mammogram report to help when comparing to future mammograms.Probably benign finding – Follow-up in a short time frame is suggested
The findings in this category have a very high chance (greater than 98%) of being benign (not cancer). The findings are not expected to change over time. But since it’s not proven benign, it’s helpful to see if the area in question does change over time. Follow-up with repeat imaging is usually done in 6 months and regularly after that until the finding is known to be stable (usually at least 2 years). This approach helps avoid unnecessary biopsies, but if the area does change over time, it still allows for early diagnosis.Suspicious abnormality – Biopsy recommended
Findings do not definitely look like cancer but could be cancer. The radiologist is concerned enough to recommend a biopsy.Highly suggestive of malignancy – Biopsy recommended
The findings look like cancer and have a high chance (at least 95%) of being cancer. Biopsy recommended.Known biopsy-proven malignancy – Appropriate action should be taken
This category is only used for findings on a mammogram that have already been shown to be cancer by a previous biopsy. Mammograms may be used in this way to see how well the cancer is responding to treatment. Some cancers are often made to shrink using chemotherapy to later be removed by a surgeon.Information from ACR, American College of Radiology, and the American Cancer Society.
Frequently asked questions
Did you know?
The National Cancer Institute (NCI) adds that women who have had breast cancer and those who are at increased risk due to a genetic history of breast cancer should seek expert medical advice about whether they should begin screening before age 40 and about the frequency of screening.