Desert ImagingThe women's center
The Women's Center
Desert Imaging has opened its newest addition, The Women's Center at Desert Imaging. We care so much about our patients experience and privacy. What was once a dream is now a reality. We offer Breast services, Ultrasound and Bone density in a beautiful and comfortable location.
Schedule your exam with us today by calling (915) 577-0100
Located at 122 W.Castellano, El Paso TX 79912.

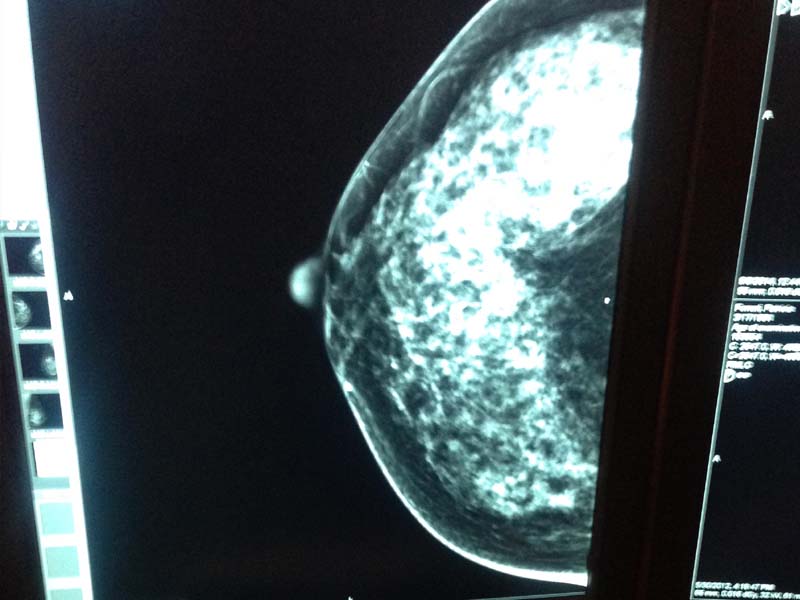
Full Field Digital Mammography
At Desert Imaging, we are all about Mammography. We only use full field digital mammography which is the Gold Standard because the image quality is unsurpassed. At Desert Imaging, all 3 stand alone locations and all our MOM Units, (Mammos on the Move, Mobile Mammogam Coaches) use Hologic Selenia.
Insurance
Most insurances cover mammography at 100%, no cost to you. The diagnostic mammogram, however, will be charged the copayment or the deductible.

Screening mammogram
A screening mammogram is comprised of 4 images, 2 of the right breast and 2 of the left. The screening images can show the radiologist if the breast is free of calcifications or mass structures. The radiologist can tell if the mammogram is normal (negative) or benign (may have cysts, masses, or calcifications that are not suspicious).
Diagnostic mammogram
A diagnostic mammogram is needed if the radiologist needs to take a closer look at cysts, masses, or calcifications that look suspicious. These diagnostic images can help the radiologist tell if something is malignant or not. If they are still questionable, a biopsy might be ordered to look directly at the tissue.
What you should know about
HENDA'S LAW
What is Henda's Law & how does it affect my mammogram?
Henda's Law is the informal name for a House Bill passed by Texas Legislature that requires mammography providers to inform women that dense breast tissue can affect the accuracy of a mammogram in detecting breast cancer.The bill was initiated by Henda Salmeron, whose breast cancer went undetected because routine mammograms did not pick up the cancerous tumors hiding behind her dense breast tissue. Women, like Henda, who have dense breast tissue may benefit from supplemental screening.
Do I have dense breast tissue?
Breast density refers to the amount or ratio of fibroglandular to fatty tissue. As a woman ages, fibroglandular tissue is replaced by an increase in fatty tissue and thus making breast cancer more readily visualized on a mammogram.

How will this affect my annual exam?
If a physician notices you have dense breast tissue, additional exams such as ultrasound may be ordered to rule out the possibility of any hidden tumors. However, it is important that you know insurance may not cover these additional screenings at 100%.
BIRADS
The American College of Radiology (ACR) came up with a standard way to describe mammogram findings and results. In this system, the results are sorted into categories numbered 0 through 6. This system is called the Breast Imaging Reporting and Data System (BI-RADS). Having a standard way of reporting mammogram results lets doctors use the same words and terms, which can help ensure better follow up of suspicious findings. These categories are used in the official report that goes to your doctor. Different wording may be used in the letters sent to patients. Here’s a brief review of the categories:
Additional imaging evaluation and/or comparison to prior mammograms is needed.
This means a possible abnormality may not be clearly seen or defined and more tests are needed, such as the use of spot compression (applying compression to a smaller area when doing the mammogram), magnified views, special mammogram views, or ultrasound. This may also suggest that the mammogram should be compared with older ones to see if there have been changes in the area over time.Negative
There’s no significant abnormality to report. The breasts look the same (they are symmetrical) with no masses (lumps), distorted structures, or suspicious calcifications.Benign (non-cancerous) finding
The radiologist describes a finding to be benign, when he/she sees benign, non malignant, structures such as, calcifications, lymph nodes in the breast, benign cysts or calcified fibroadenomas. This ensures that others who look at the mammogram will not misinterpret the benign finding as suspicious. This finding is recorded in the mammogram report to help when comparing to future mammograms.Probably benign finding – Follow-up in a short time frame is suggested
The findings in this category have a very high chance (greater than 98%) of being benign (not cancer). The findings are not expected to change over time. But since it’s not proven benign, it’s helpful to see if the area in question does change over time. Follow-up with repeat imaging is usually done in 6 months and regularly after that until the finding is known to be stable (usually at least 2 years). This approach helps avoid unnecessary biopsies, but if the area does change over time, it still allows for early diagnosis.Suspicious abnormality – Biopsy recommended
Findings do not definitely look like cancer but could be cancer. The radiologist is concerned enough to recommend a biopsy.Highly suggestive of malignancy – Biopsy recommended
The findings look like cancer and have a high chance (at least 95%) of being cancer. Biopsy recommended.Known biopsy-proven malignancy – Appropriate action should be taken
This category is only used for findings on a mammogram that have already been shown to be cancer by a previous biopsy. Mammograms may be used in this way to see how well the cancer is responding to treatment. Some cancers are often made to shrink using chemotherapy to later be removed by a surgeon.Information from ACR, American College of Radiology, and the American Cancer Society.
Frequently asked questions
Did you know?
The National Cancer Institute (NCI) adds that women who have had breast cancer and those who are at increased risk due to a genetic history of breast cancer should seek expert medical advice about whether they should begin screening before age 40 and about the frequency of screening.